How do physicians prioritize?
Michael 2018; 15: 64–69.
A selection of physicians in the Oslo University Hospital (OUH) in Norway responded to a survey of how they did prioritize patients received for consultation and/or treatment. They were given a choice of seven statements. Their importance for the prioritizing was weighted on a scale from one (low) to six (high). Patients defined with the right to treatment came out on top, while financial refunding as compared to resources used, received the lowest score. There was no difference between consultants and physicians in training or between physicians from medicine and surgery departments.
Introduction
DRG (diagnosis-related-groups) and activity based financing were introduced to Norwegian hospitals in 1997 (1). Particularly in the beginning, the debate was intense about how this system affected physicians’ choices. Would the financial reimbursement influence the medical decisions in an unwanted way (2, 3)?
Classical economics presuppose that an economic man is maximizing his utility function, reacting to economic incentives. As a physician inside a hospital, he would prioritize patients where financial funding compared to resources used had the best ratio.
There have been many statements that this is not necessarily a realistic and correct foundation for an analysis. Simon (4) declares that there is nothing like a rational economic man. He may be «intendedly rational but only limited so.» A rational decision presupposes full and equal information. Particularly in the health services there is neither complete nor equal information between the actors in the game. There is an asymmetry of information (5). Stiglitz in his prize lecture on information economics goes even further. (6) «.., while much of the earlier literature focused on simple situations of information asymmetry – …………., the problems of information imperfections run deeper,..».
One way of coming closer to analyze what to expect from an activity based system, is to ask those deciding how they prioritize. This was done in this survey in the beginning of 2016, as part of a larger study about physician activity.
Methods
A questionnaire to individual physicians was used. The physicians worked in a part of Oslo University Hospital (OUH) encompassing 40 percent of the hospital’s patients, covering both surgical and medical specialities, consultants and residents (physicians in training).
Physicians in these three clinics of Oslo University Hospital (OUH) received the questionnaire:
Clinic for head, neck and reconstructive surgery, comprising the departments of ear-nose and throat, ophthalmology, oral-maxillofacial surgery and plastic surgery.
Clinic for orthopaedics
The neuro clinic, comprising neuro medicine, neurosurgery, the national centre of epilepsy, the department of psychosomatics, the department of physical medicine and rehabilitation, the department of neuro habilitation.
To promote the questionnaire, it was first presented for all departments in a management meeting with the heads of all departments. Then it was presented in the physicians’ morning meeting, except for orthopaedics and neurosurgeons. The questionnaire was then distributed electronically by the department managers or in a paper version to every individual physician working in the department. 167 physicians answered the questionnaire. Of these 154 (92 %) answered the questions concerning how they prioritized between patients.
The patient was characterized by seven parameters and the physicians should give each a number from 1–6, telling the importance it had. One was the lowest and six the highest score of importance. The characteristics were:
Patient defined with the right to treatment (Right to treatment)
Assumed health benefit by the consultation/treatment (Assumed health benefit)
Assumed reduced loss of health
How long the patient had been waiting (Time waited)
Health status of the patient (Health status)
Resources needed for the consultation/treatment (Resources needed)
Financial reimbursement
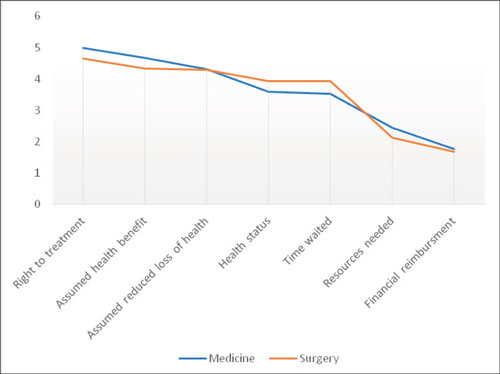
Figure 1: How physician prioritize patients for treatment/examination, medicine and surgical departments.
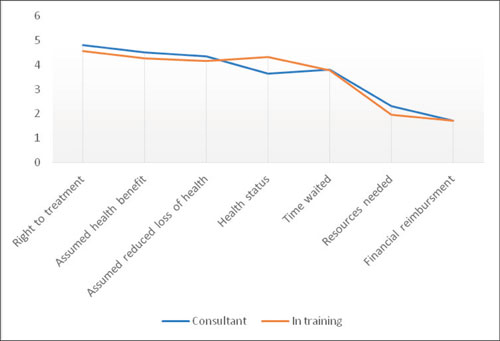
Figure 2: How physicians prioritize patients for treatment/examination, consultants and physicians in training
Norwegian patients have the right to treatment according to a secondary law* Secondary law about prioritizing health services, right to necessary health support from specialist health services, right to be treated abroad and … § 2 and §2a. Authority in law: Law about patient rights and users’ rights..The Health directorate has guidelines for 33 medical groups, each describing different conditions. Assumed benefits of treatment are compared to the expected costs. Defined medical conditions are entitled to treatment within a certain time span. If this is not given, the patient may seek treatment from another hospital, and the original hospital must pay the bill.
Results
The results are first presented for physicians from medical and surgical departments. There is hardly any difference between physicians from the two main specialties, as to what they emphasize. Highest ranking is given to patients defined with the right to treatment. Only looking on financial reimbursement is given the lowest rating. The standard deviation is about 1/3 for the five highest rated criteria, while the deviation rises to about 0,6 for the two lowest. The variations in how the physicians emphasize the criteria are larger in how they assess resources needed and financial reimbursement, than for the other criteria. The standard deviation is smaller for medical physicians than for surgeons.
The picture is very much the same when consultants and physicians in training (residents) are compared. They do not differ much, and the slope of the curve is almost identical in the two figures, with a small deviation for general condition and time waited. Right to treatment is rated highest and financial reimbursement lowest. The standard deviation for the two groups is almost equal, except for how they evaluate resources needed and financial reimbursement. For these two the standard deviation is higher for consultants than for physicians in training.
Discussion
From the beginning, the intention behind activity based financing of Norwegian hospital services is to be neutral, related to different illnesses and treatments. The income should balance the estimated costs, so no treatment should be more profitable than others. Despite this, both the Health directorate (7) and the Norwegian Medical Association (8)are skeptical and afraid that the financial solution is creating a situation where what is paid, comes before what is needed.
It is interesting that the respondents in this survey have «patients with the right to treatment» as the highest rated criteria for selection, and financial reimbursement as the lowest criteria. I will draw the attention towards two reasons which might explain this:
Patients with the right to treatment have been selected in a process where medical benefits and resources used are evaluated together. The hidden threat is that the patient will be treated elsewhere for the cost of the physician’s hospital, if she or he is not prioritized. Assuming the costs connected to the particular treatment process are equal in different Norwegian hospitals, the loss of the first hospital is the loss of activity based income for those cases which the physicians evaluates the lowest when prioritizing. The criterion with second highest score was the estimated health gain by the treatment, indicating that their embracement of «patients with the right to treatment» is because they find this statement as a help in their medical evaluation.
The second interesting point is that the physicians have a public set of indications as their top priority tool. Studies have documented that physicians are skeptical to rules enforced on their practice from central bodies (9). Answers to this survey indicate that there are situations where this skepticism is traded for acceptance. One reason could be that the «right to treatment» is not mandatory. The Health directorate have written guidelines for different specialties, and there is a room for physician assessment.
Conclusion
We should not be too surprised to see physicians giving resources used and financial reimbursement a low rating as criteria for prioritizing. Norwegian hospital physicians have no direct incentive to be concerned about the hospital economy when making decisions upon what to do for a particular patient. The daily and normal, micro decisions, are probably taken separately from a discussion of the hospital budget. Such appraisals could come to the surface with a situation where a treatment could be very expensive, beyond what is normal, a situation which, however, only occasionally occurs.
What may be surprising is that criteria for prioritizing, developed publicly, obviously have been embraced by the physicians. That opens for a study to see if the results would be repeated, and to find out more about what supports this impression.
References
DRG historie i Norge fra slutten av 70-tallet: Health Directorate of Norway; 2017 [Available from: http://sites.helsedirektoratet.no/finansiering/drg/drg-struktur/Sider/drg-historie- i-norge-fra-slutten-av-70-tallet.aspx.
Riksrevisjonen. Riksrevisjonens undersøkelse av effektivitet i sykehus – en sammenligning av organiseringen av hofteoperasjoner. Oslo: Riksrevisjonen; 2003 14. November 2003. Contract No.: Dokument 3:3 2003–2004.
Hansen TWR. Underkoding er vanligere enn overkoding. Tidsskr nor legeforen 2005; 125 (16):2244.
Simon HA. Administrative Behavior. 5th ed. New York: The Free Press; 1997: 368.
Arrow K. Uncertainty and the Welfare Economics of Medical Care. The American Economic Review. 1963; 53 (5):941–73.
Stiglitz JE. Information and the change in the paradigm in economics. In: Columbia Business School CU, Prize Lecture 2001: 68.
7. Utviklingstrekk i helse- og sosialsektoren 2007. Oslo: Sosial- og helsedirektoratet; May, 2007. Report No.: IS-1443.
8. Lang, lang rekke – hvem skal vente, hvem skal få? Rapport. Oslo: Den norske legeforening; 2007.
Martinussen PEF, Jan C. Vrangbæk, Karsten. Magnussen, Jon. Organisatoriske forhold og løsninger i spesialisthelsetjenesten – hva mener legene? Michael. 2017;14, Supplement 19:11.
Jostein Holte
tarald.rohde@sintef.no
