The grandmother approach: Teaching medical students medical history – some personal experiences* Revised, abbreviated and updated version of a keynote lecture given at the XXII Nordic Conference on Medical History in Bergen 3.-6.6.2009 (Title of keynote: Teaching medical students medical history; Necessities and challenges). Some of the topics in the lecture dealt with medical teaching in general, particularly at the University of Oslo. These have been further elaborated on and are published in: Larsen Ø. The winds from Maastricht – some personal reflections on teaching medicine at the University of Oslo. Michael Quarterly 2011; 8: 329-43, and have therefore been omitted or tuned down here.
Michael Quarterly 2011;8:499–513.
Experiences from a long-time commitment in teaching medical history have shown that teaching medical students needs some special considerations because it means conveying historical knowledge to a target group whose main motivation is to learn medicine for their future professional life. The objective is to convey to them the ability to allow time and space perspectives into their medical thinking. Therefore, the teaching has to be tailored by means of: (1) an appropriate choice of topics covered by (2) the most suitable teacher. The (3) audience of students should be at an optimal point on their way through the curriculum. The (4) most effective teaching methods should be carefully selected, and one should see to that medical history fits into the general (5) teaching climate of the faculty in an integrated way.
Some experiences gathered from an approximate 45-year engagement in teaching medical students medical history might be of interest to others in the field. During my years of service, some personal views on aims, methods and means in teaching medical history to a quite special audience have inevitably emerged, in which tailored messages are required – for the medical students.* As I have been occupied with teaching challenges for so long, I have written about it in various books and articles. In footnotes here, I therefore refer to writings in which the interested reader may find more extensive comments on topics taken up in this paper. (I started as a research fellow in medical history at the Institute of Hygiene of the University of Oslo in 1964 and am still teaching at the successor of this institute, the Institute of Health and Society.) From 1971 to 1977, I also taught medical history on a part-time basis at the University of Tromsø, and taught public health as a professor in preventive medicine in Tromsø 1976-77. Since 1998, I have given lectures in medical history at NTNU, the University for Technology and Natural Sciences at Trondheim, and for some time since 2008 at a public health course at UMB, the Norwegian University for Life Siences in Ås.)
An example: Many years ago, I introduced my «grandmother trick»* Magne Nylenna refers to it in his article, Formidlingens kunst. Michael 2008;5:175-9.. It works! Imagine that you are a university teacher standing in the lecture room in front of a new class of students. They are medical students at some stage of their six-year-curriculum, which is how we do it in Norway. The first challenge you will encounter appears immediately, and it is typically Norwegian: They are highly selected for their intellectual abilities. For example, at the University of Oslo less than one out of 10 applicants is accepted.* In 2008, there were 1,139 applicants to Norwegian medical faculties who indicated the University of Oslo as their first choice. A total of 105 places were available. (Universitas 2009;63:#13, 4-5.) That means that these sparkling minds will instantly disclose any weak argument in your presentation, so be careful! But the upside to this is that they will also know to duly appreciate a well-balanced and meticulously prepared lecture.
But how to start? How to grasp their interest at the very beginning and make them your partners in setting a stage in which they see their position as future medical personnel with a perspective in both time and space?
When silence has settled over the room and the eyes of the expectant group are turned towards you, make a short but noticeable rhetorical pause, point at one of the students and simply say: I know something about your grandmother! The surprised student will look at you with a question mark, while the others are wondering what will happen next.
Beforehand, you have made some calculations: This 20-year-old student will probably have a grandmother who was born some 75 to 80 years ago. For the time being (2011), this means in the early 1930s. From your own command of medical and social history, you know fairly well how the life and health of a female from that cohort generally was and is. Therefore, you will not make any large mistakes if you start telling a story about probable traits regarding her growing up in the 1930s, about her enduring rationing and nutrition problems during the war years, about her later embarking on an educational track, e.g. two or three years to become a school teacher or a nurse, before marrying in her early 20s in the 1950s.
You will be able to talk quite confidently about her health. You may for example suppose that she was regularly summoned by the health authorities to be checked to disclose any tuberculosis infection, that as a child she suffered from pneumonia, which scared the whole family because no effective drug was available at the time. From your demographic knowledge, you may assume that her summer vacations were spent on the family farm out in the countryside where her ancestors originally came from, and that these summers included weeks of diarrhoea and infected bruises on her knees etc., etc.
While listening, the student will sometimes nod affirmatively, sometimes shake his/her head and object that it was not exactly like that. But anyhow, the student has to admit that the description fits quite well at large.
Then your question to the audience is: How do I know all this? That is young friends, this is what you also will know when you are proficient in medical history!
You can see in their eyes that by now you have them in the palm of your hand.
You then proceed to the next questions: Have any of you been to a medical ward in a hospital? Even if they are young, many of them have invariably had a summer job in a health institution when thinking about applying to medical school. What sort of patients did you see there?
Their faces open up: They realize that the ward was dominated by grandmothers! Now the time has come for your conclusion: You point out to them that with a command of medical and social history, they will be well prepared to not only communicate with their grandmother’s generation, but to also understand their patients’ backgrounds, their attitudes – and their relationship to health personnel, to you, dear students!
The grandmother trick, or a similar setup, is hereby recommended!
Prerequisites for teaching
If a teaching situation is to be successful, the most important element of course is: (1) the topic. The next element is (2) the teacher. As a teacher, you just have launched a topic that has been accepted, found to be relevant and interesting by your (3) audience. In the example described above, the (4) teaching method chosen for communicating the topic from the teacher to the students is that of a lecture.
But in addition there is a fifth element, which we can call (5) the teaching climate. This includes the integration of the discipline, in this case medical history, into the curriculum, into the general objectives of the faculty, into the self-image maintained by the profession, and last but not least, into the knowledge and skills which are expected from the candidates by the public.
Successful teaching depends on control of and harmony between these five elements:
(1) Relevant topics
The context of the grandmothers in the hospital wards is only one example of the relevant topics; there of course is a series of others. When established, The Nordic Association for Medical History took up the discussion of relevant topics as one of its first tasks.* The idea of a Nordic Association was discussed at the V. Nordic Congress for Medical History in Helsinki in June 1975. The Finnish association Amici Historiae Medicinae under its chairman, professor Harald Teir, had taken the initiative. A preparatory meeting was held at the Medical Museum in Copenhagen in December 1975, and the Association was formally constituted in a meeting at the Medical Museum in Stockholm on March 27, 1976, with nine Nordic associations for medical history represented. On September 30. and October 1, 1976, a symposium on teaching medical history was held at the Lysebu Conference Centre in Oslo in connection with a meeting of the Nordic Federation for Medical Teaching. (See: S(trandberg) H. (Introduction) in: Larsen Ø. (red.) Medisinhistoriske emner i medisinsk undervisning. Tromsø: Institutt for samfunnsmedisin, 1976. 2. ed.) In the autumn of 1976, 29 scholars and students from the Nordic countries and Germany gathered at a symposium in Oslo in order to discuss, and agree upon, what a framework for medical historical teaching should look like.* The participants were: Bente Alver, Anne Sofie Brønn, Lasse Efskind, Erik Falkum, Bente Gauslaa, Andreas Grimeland, Ejnar Hovesen, Arthur E. Imhof, Lorentz M. Irgens, Jørgen Koch, Wolfram Kock, Einar Kringlen, Ingegerd Frøyshov Larsen, Øivind Larsen, Laurits Lauridsen, Eddie Lidén, Bengt I. Lindskog, Kari Martinsen, Lauri O. Meurman, Arne Næss, Ingela Ohlin, Tomas Riesenfeld, Sam Schulman, Hindrik Strandberg, Harald Teir, Inger Wikström-Haugen, Odd Wormnæs, Lars Öberg and Bjørn Østberg.
In the discussions, science history aspects were taken up, in addition to the history of medicine and so forth. The use of medical history in the teaching of medical nomenclature was also taken in. However, a special emphasis was put on the context-oriented medical history, in which a seamless connection to the general objectives of the medical curricula was described. Demography, the history of diseases and social history include highly relevant elements. Folk medicine in a wide sense, including changing attitudes toward health and disease, was also highlighted.* See Larsen Ø. (red.) Medisinhistoriske emner i medisinsk undervisning. Tromsø: Institutt for samfunnsmedisin, 1976. 2. ed. The booklet includes surveys of medical historical teaching in the Nordic countries up to 1976.,* In 1979, the Nordic congress for medical history in Oslo had attitudes against diseases as its main theme. See Larsen Ø. (red.) Synet på sykdom. Oslo: Universitetet i Oslo, 1979, 2. ed. A recommendation following these guidelines was presented to the Nordic medical faculties through the Nordic Federation for Medical Teaching.
In Norway, and especially in Oslo, these principles have been followed since 1971 in various forms, according to the shifting setup of the medical curriculum in general. The strongly context-linked topics have been shown to integrate quite well into the general curriculum.* See Larsen Ø. Learning medical history in Oslo: Training for medical practice. Croatian Medical Journal 1999; 40(1):29-33.
In the 1970s historical aspects from six fields were covered in Oslo and Tromsø: (1) What is health and disease? (2) Health and culture, (3) Medical thinking in history, (4) Measuring of health, (5) Environment with influence on health, and (6) Health conditions affecting the social environment.* In the 1970s, teaching in the new discipline of Behavioural science in medicine was gradually introduced in Oslo, with e.g. some sociological topics previously taught in medical history being taken over by teachers from behavioural medicine.
In the 1990s, the following subjects were taught in Oslo: (1) The development of the medical profession, (2) Primary health care history, (3) Diseases, demography and health services in Norway from the 18th century onwards, (4) The development of medical science – blood circulation as an example, (5) The history of psychiatry, and (6) Extinct and living Norwegian folk medicine.
A newer topic which has proven to be a good entry to medical historical thinking and to context orientation in general in Oslo is a series of lectures on medicine and arts,* Larsen IF. Medisinens menneskelige ansikt – bildende kunst. T. norske Lægeforen. 2000; 120: 3762-4. See also Frich JC. Undervisning i medisin og kunst – hvilket utbytte har studentene? Michael 2008;5:245-54. including literature, music and architecture. This is comprised of a survey over medical motifs in Norwegian visual arts, with an additional lecture on the painter Edvard Munch (1863–1944) and his relationship to health and disease, which has been positively perceived by the students.
The relationship between architecture and health in history has considerable relevance when teaching housing hygiene during the public health term.* While general medical historical topics are most easily taught relatively early in the six year curriculum, is the experience that housing history is felt most relevant by the students at the end of the curriculum – possibly also because they at this stage have been on the housing market themselves.
(2) The teacher
Teachers in medical history are frequently academics with a medical background and an additional training in medical history. However, teachers are also often historians with a special command of medical history. What works best is an open question, though as a rule highly is dependent on the persons in charge. A combination of teachers with various backgrounds participating in the lecture series is an ideal situation. It may also be sensed that a language problem is lurking in the background. The professional language of, e.g. some social scientists, may sound like ringing bells to more grass-roots prone medical students. My key point is that the teachers should understand the professional traits of the disciplines involved. An historian who does not get under the skin of the doctors has the same handicap as a doctor who has not internalized the working methods and reasoning of the historians. Nonetheless, there is no sense here in stirring up the sometimes sleeping, sometimes open discussion as to whose field medical history belongs.
Medical history opens up for views on the relationship between health, science and society in a broader sense. Therefore, medical history may be perceived as provoking, and as such even has the potential to influence the development of, say, the role of the doctor and the setup of the health care system. Thus, the orientation and abilities of the teacher will be important.
One issue, however, is crucial: The ability to convey the topic in such a way that it is felt more or less as a necessity by the students to help fill a hole in their knowledge. The teacher should present the message as is done in anatomy or pathology, in which the use of high magnification lenses is supplemented by a low magnification survey. Medical history teaching is like switching in the low magnification on the microscope turret, and then subsequently putting the detailed information into its context.
The main objective of the teacher is to teach, not to preach.
(3) The audience
This text deals with the teaching of medical students. Here, one should make an effort to place the teaching of medical history on the correct level in the curriculum. Where that is may be different in different medical schools, but the point is that the students on the one hand should be so socialized into medicine that they already have a professional identity. On the other hand, they should not be so high up in their study years that the scary prospect of the final medical examination is the only issue that fills their heads.
However, groups other than medical students also have a need for medical historical knowledge. Many a teacher in medical history will have had experiences with other categories of students. The common lesson learned will be that each group probably has its own attitudes and own expectations for the teaching, and that a quite deep concern about this fact is required to make the teaching successful.* From 1971, and in some years onward, the University of Tromsø offered a one-year course called Basic Medicine (“Medisin grunnfag”) to applicants from the social sciences, persons from the social security system, students who aimed at a position in health administration, etc. At least in the first years, medical history here had a strong position with a series of approximately 50 lectures. The reception by the audience was good, as many of the listeners were quite seasoned and had a considerable amount of life experience as background for reflexion. Science history should have its unquestioned place in postgraduate research training programmes, as well as the history of health and disease in programmes in international and global health. For example, in nursing schools medical history being used as a tool to strengthen professional pride and professional ties is quite common. When I taught medical history in a high school for librarians, the knowledge to facilitate orientation in old literature was of course the special point of view held by the students. And to teach medical history at a so-called «university for the elderly» gives the lecturer a special, yet useful challenge, when confronted with the life experiences present in the lecture room!
Experience with teaching different groups is an asset because the need for adjusting to the audience clearly comes into view.
(4) Teaching methods
Personally, I think that the old-fashioned lecture still holds many virtues as an effective way to transfer medical history knowledge. I have no documentation behind this opinion other than my own experiences, listening to other teachers and giving lectures myself. Since context is the keyword, a well-composed lecture can give the audience a survey fit for further studies, as interest and curiosity may be awakened. Group work, etc. may be good for special topics, but it is more time consuming, may weigh heavily on the motivation in teachers and students over time, in addition to also blurring the perception of context.
What sort of audiovisual equipment is best for teaching medical history? I think there is a danger in making the teaching and the topic too exotic, in that you run the risk of setting up a distance between the context in time and place that you want to convey, as well as the reality in which the students are.
In the lecture situation, it may be wise to only use slides and other aides with caution, and only when a clear message is being conveyed. This way, the means are not allowed to distract from the message. Old photographs may well give documentation, but they may also constitute an unwanted distance. The grainy black-and-white mood in an old picture, showing people with strange clothing and haircuts, gives connotations that may be misleading and disturb what you want to say to people who are not used to penetrating such historical filters.
At least to me over the years, the oral presentation in front of a large blackboard, with an abundance of chalk at hand, has proven to be the audiovisual winner. Arguments evolving in white letters on the board, and being written down in the notebooks of the students, hold the pedagogic position. The students should learn that the past and its surroundings are not a foreign world that they make entertaining excursions into, the past is part of this world.
The students should learn that they live and work with ties to the realm of their grandmother’s generation. To a large extent, the living conditions of the population today have been shaped by planners now resting in their graves. And the society of their own grandchildren will depend on attitudes held, and future decisions made, by the students themselves. These facts make medical history important to them.
The weight on context in time and place should also address the topic of shifting attitudes within the same time and place framework. From the very first day of a modern Norwegian medical curriculum, the students learn that medical practice should lean on evidence-based knowledge, which of course is correct. In contrast, they must also learn that there are other attitudes to life and other realities that may hold the same importance. Other forms of knowledge are around, and serve as background for decisions of many types.
In a clinical situation, it can be difficult to explain to one of the grandmothers that putting cat fur on her back will not necessarily work on her pain, even if she claims that her neighbour was totally cured in that way.
Popular and professional perceptions of evidence are different, and this fact must be taken into consideration.
In professional medicine, treatment based on the impressionistic «doctor’s experience» still exists, and differences between outcomes of treatment in different hospital wards can probably also be interpreted that way, which is an interesting issue for discussion.
When the historical approach is used for public health topics,* In the current public health textbook used in public health in Norway, these factors are discussed more extensively. (Larsen Ø, Alvik A, Hagestad K, Nylenna M. (eds.) Samfunnsmedisin. Oslo: Gyldendal akademisk, 2008.) it is important to stress by means of examples that medical knowledge comprises only one set of arguments and bases for decisions, e.g. with cultural traditions, political programmes or personal beliefs being important as well. Meanings and opinions not based on knowledge, and held by key persons and politicians, are often fully accepted as background when important decisions are settled. Here, the medical historian carries a special and important responsibility. In many parts of the Western world, the health services and welfare state institutions are under attack for reasons of cost saving, pursuit of liberalistic ideologies, etc. Most people involved in these discussions will be so young that they have no personal experience with the old society where this modern security net is lacking. Therefore, teaching about health, medicine and social conditions in earlier times may serve as an important eye-opener. Group studies, theses and so forth with materials from Norway in the period up to World War II may render results with practical bearings.
For curricula in which written theses of various sizes are required, topics from medical history can be well suited. In Norway, we have an abundant amount of archival material on the public health situation, e.g. reports written on an annual basis by the district’s physicians. A well delimited topic for a student thesis may very well be set up based on this type material.
It is also necessary to find suitable examples to underscore the fact that for many people health is only one valid value among other values, and that the ranking of values change in time and place. As one example, a picture of some old psychiatric treatment procedure from the times before effective drug treatments were available, may be used as point of origin for a useful discussion of the necessity of looking upon history in context. A so-called long-bath* An example is the “long-bath” equipment from the medical historical museum in Stockholm. See Larsen Ø. Kulturelt akseptabel tvang. Tidsskr Nor Lægeforen 2002;122:1962. or a straitjacket from an old asylum should not immediately be regarded as inhumane or cruel. An understanding of the total situation of the time should be drawn up for the students, given other cultural standards ruling the use of restraint on the one hand, and the difficult task of controlling violent and dangerous patients in the pre-medication era on the other. A general discussion of the development of the perception of human rights could, if felt to be appropriate, follow in the wake. Examples such as this should also be used as a warning against cheap, populistic dives into medical history.
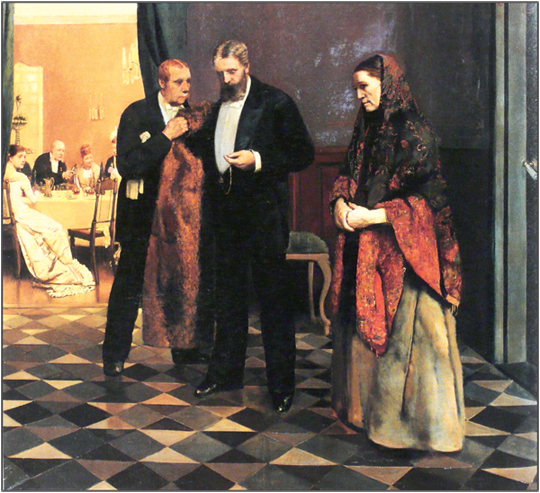
Figure 1: Bud efter Lægen (1881–1882) by Christian Krohg (1852–1925). (Oil on canvas. Trondhjems Kunstforening)
(Photo: Ø. Larsen)
To use pieces of art as an entry point may be useful. A painting such as Bud efter lægen (1881–1882) (Calling for the doctor) by Christian Krohg (1852–1925) can illustrate several issues – from the class differences in a capitalist society to the humble respect for the doctor in the past.* See Larsen Ø. Legestudent i hovedstaden. Oslo: Gyldendal Akademisk, 2002. (Figure 1.)
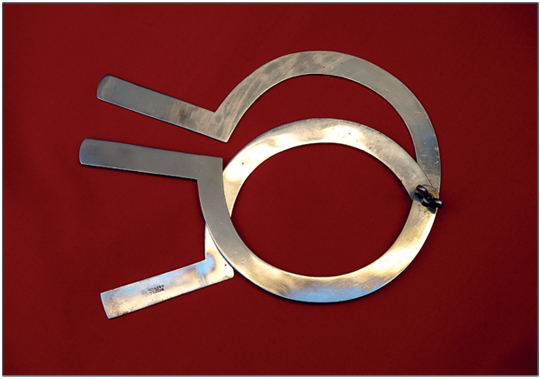
Figure 2: Amputator for female breasts, last decades of the 18th century. (Section for medical anthropology and medical history, University of Oslo)
(Photo: Ø. Larsen)
I will probably surprise some of my readers by saying that I do not recommend museum visits as part of the teaching in medical history in the first place. Many museums present information taken out of context, or at least alienated from it. And nowadays, many museums primarily aim at reaching schoolchildren in their presentations, cleverly enough, although this approach may be disturbing to a mature student. What students learn in museum presentations has to come as a supplement when their command of the context is satisfactory.
However, the passing around in the classroom of an old surgical instrument may give the opportunity to stress the connection between the item and its context. An 18th century breast amputator (Figure 2) cannot be understood without looking into its clinical context, and may therefore serve well as a pedagogic tool.* Larsen Ø. Brystamputasjon – brutal eller skånsom? Tidsskr Nor Lægeforen 1987;107;VVII. This device effectively demonstrates the necessary techniques in the pre-anaesthetic era, when swift surgery was the most merciful to the patient. And a picture of a living leech can illustrate that an obsolete method is not necessarily obsolete in another context, as leeches are still used today in hand surgery.* Larsen Ø. Blodiglen – en medarbeider i aksjon. Tidsskr Nor Lægeforen 1991;111:2231-3.
Is it possible to make excursions into history? Yes, it is. Because societies develop at different paces, it is possible to learn about the past by visiting other societies. Excursions to exotic developing countries may be useful in this respect, even though in the years from 1995 to 2001 we had an annual four-week student training programme in not-so-exotic Latvia for groups of students from Oslo. At that time, Latvia was changing from a Soviet style of medicine, and had many traits in common with Norwegian medicine and Norwegian health conditions a generation earlier. In the hospitals, other caring principles could be observed, as well as other stages of diseases than what they were used to seeing, and even strange diseases such as diphtheria and leprosy.
From a 1996 parallel, collaborating student groups were deployed to La Crosse, Wisconsin in the US. On returning, they were supposed to write a report on a medical topic which they had studied and compare what they had learned in Latvia, the US and Norway. This outplacement proved to be very successful and resulted in 12 interesting comparative reports over the years. Concentrating on public health and contemporary medical history, the students really had been on an excursion in time and place.* See Larsen Ø, Kilkuts G. Health in Latvia 1991-2004; Years of conflicting values. Michael 2005; 2: Suppl 1. About the outplacement system in general, see Larsen Ø. Administrativ organisering og akademisk virke – Institutt for allmenn- og samfunnsmedisin ved Universitetet i Oslo. Michael Quarterly 2011; Suppl. 10. Nonetheless, the situation changed rapidly, and Latvia had more or less approached Western European standards after 2001, and the pedagogic point of staying there became less visible.
The large medical museum in Riga was at least in the 1990’s rather oldfashioned, but its wide-ranging exhibitions from pathological specimens to space medicine equipment could be thought provoking. Medical practice, not unlike earlier times in Norway, also is exhibited. The exhibition on Demikhov’s transplantation experiments touch on problems of research ethics* Larsen Ø. En forskningshund eller to. Tidsskr Nor Lægeforen 2000;120:3366.. (Figure 3).
(5) The teaching climate
In 1996, a major change took place in the medical faculty at the University of Oslo, as a totally new curriculum* “Oslo -96”. See: Larsen Ø. Legestudent i hovedstaden. Oslo: Gyldendal, 2002. was introduced. The main principle from now on was the so-called Problem Based Learning (PBL), in which the number of lectures in all disciplines were reduced to a minimum and replaced by small student groups working under guidance with specific topics.* For further discussion of this topic, see: Larsen Ø. The winds from Maastricht. Michael Quarterly 2011; 8: 329-43.

Figure 3: A case for discussing laboratory ethics: A two-headed dog from the transplantation experiments by the Russian researcher Vladimir Petrovich Demikhov (1916–98), stuffed and on exhibition in the medical museum of Riga.
(Photo: Ø. Larsen)
While topics in medical history had previously been presented in a conventional series of 24–30 lectures, one had to concentrate in the new curriculum. Topics deserving to be highlighted were the development of public health, medical teaching and the role of the doctor, the medical profession and the development of infectious diseases. A PBL topic on tuberculosis was followed up by a keynote lecture on infections.* Since 2007 given by the specialist in Robert Koch (1843-1910) and history of infectious diseases, prof. Christoph Gradmann. For a discipline such as medical history, more conventional approaches have been felt to be better because it then is easier to raise the eyes of the students from singular problems to the general context, and make them slowly digest what they learn.
What about the doctor’s role in the historical setting? An example: When the district physician, Marius Brostrup Müller (1841–1908), suddenly died from a heart attack during a strenuous travel to a house call, an enormous monument was erected by the municipality and his friends on the site where he expired. This was not only because of his work as a beloved doctor. But because he had also been an eager promoter of modernizing and developing the local society he was a part of.* Larsen Ø. Endret rolle i samfunnet. Tidsskr Nor Lægeforen 1990;110:2733.
We have already touched on the ever ongoing discussions as to the role of the doctor in society. Should she or he be concentrated on the practical treatment of diseases and injuries? Or should the doctor have a wider perspective, including a responsibility for society as a whole in health matters? Should the doctor be a health worker or a health provider?* The relationship between the images of the doctor (the life saver, the caring supporter, the gate-keeper) and the objectives of the doctor (serve the sick, serve the society, serve the science, serve yourself) is the main topic and have been discussed in depth in Larsen Ø. (ed.) The shaping of a profession. Canton MA: Science History Publications/USA, 1996. As waves are rolling in this discussion, headwinds and tailwinds may be experienced when teaching medical history – and also when teaching public health. The perspective affects the proneness to take in contextual knowledge. The health worker ideal is more likely to focus on the individual person, and on shortsighted perspectives, than is the health provider ideal of a doctor. At the universities in Norway, the perspective orientation probably shows some variations among the faculties, as does the teaching climate for medical history.* See: Larsen Ø. The winds from Maastricht. Michael Quarterly 2011; 8: 329-43 for the appalling differences between Trondheim and Oslo.
When some students object that public health topics such as history, hygiene, public planning and other subjects dealing with health on an agglomerate level are not relevant to their future work, they are right to a certain degree because the general development in society and the medical profession has made it so. Even the re-emerging development of the discipline of social medicine, with its concentration on relief to the individuals of vulnerable groups, may be a problem for conveying a more overruling understanding of the group perspective, and for the command of context issues. To a health worker, the core system is the health care system. To the health provider, the core system may lie outside the health care system and the tools are to be found in politics, public planning, the public economy, etc. Here, the health provider needs knowledge and skills. If well integrated into a faculty and curriculum, and in a suitable teaching climate, a teacher in medical history may contribute in an important way to encompassing the future doctor in society.
But anyhow dear students, do not expect that a large monument will be raised on your grave in the modern world.
Decades of development?
Experiences from my own life in the field of medical history over the past 45 years tell me that there exists an interesting paradox. The general interest for the history of medicine, health and the social context seems to be growing steadily. This applies within both medicine and other academic fields, as well as among the general public. This fact need not be documented or elaborated on further here. But in the modern medical curricula from which the coming doctors are trained, as a rule there is only rarely space for, say, a lecture series or an intensive course in topics from medical history. Teachers in medical history simply have to adjust to the fact that the curriculum can be felt to be like a straitjacket from old psychiatry.
However, according to my experience, the simple key to success when you have medical students in your lecture room is to have in mind that what they need in the first place is to achieve the ability to include the time and space perspective in their future professional work.
Institute of Health and Society
University of Oslo
oivind.larsen@medisin.uio.no
