Atherosclerosis, inflammation and leukotrienes
Michael Quarterly 2011;8:514–22.
Atherosclerosis, which is a chronic inflammatory disease that leads to the formation of plaque on the inner lining of the arteries, is a global problem in terms of its consequences such as myocardial infarction and stroke. Although inflammation is an established factor driving the atherosclerosis process, understanding the vast complexity of the disease is crucial in designing anti-inflammatory treatments as part of the prevention of cardiovascular diseases. Proposing new ways to block inflammatory processes occurring in arteriosclerosis may be one way to operate in order to design new drugs which are adequate for the treatment and prevention of cardiovascular diseases. In asthma, a chronic inflammatory disorder that affects the airways, therapeutic agents that prevent the synthesis of leukotrienes have been shown to be an effective treatment and to also reduce inflammation in asthmatics. Therefore, inhibiting the leukotriene pathway may be a possible treatment of atherosclerosis. Leukotrienes are inflammatory mediators that are derived from the 5-lipoxygenase pathway of arachidonic acid metabolism. However, this pathway contains both pro- and antiinflammatory mediators, and a complete understanding of these pathways in atherosclerosis still remains to be established. The present review will discuss some recent advances in the understanding of the role of inflammation in atherosclerosis, with a focus on studies on leukotreiens.
Background
On a global level, cardiovascular diseases (CVDs) are the number one annual cause of mortality (1). CVDs account for approximately 16.7 million deaths each year (2), and by 2030, the number of deaths is expected to increase to almost 23.6 million (1). In 2009, 3,380 people died only from acute myocardial infarction in Norway (3). The most common reason for myocardial infarction is an underlying atherosclerosis, which causes limitations of blood flow in the coronary arteries. In addition to coronary heart diseases, patients suffering from atherosclerotic lesions are also more prone to cerebrovascular diseases, thrombosis and embolisms.
Atherosclerosis is a chronic inflammatory disease in which the construction of a plaque in the inner lining of arteries may lead to fatal consequences for a normal functioning of the human body. The process of forming this plaque is referred to as atherogenesis. The disease occurs mainly in the aorta, the carotid arteries, the coronary arteries, the iliac- and femoral arteries and other large-to medium-sized arteries (4). Atherosclerosis may arise during exposure to elevated cholesterol levels, as well as other factors that can possibly harm the arterial walls. In addition, the body’s immune system will be activated, which triggers the production of inflammatory mediators. Dysfunction of the endothelial monolayer at the inner lining of arteries may be one of the starting points in the atherosclerotic progression, as a fracture of the lining will promote the recruitment of immune cells (6). Elevated blood levels of cholesterol can also be a contributing factor to endothelial change and permeability (5).
Inflammation and atherosclerosis
Inflammation is a protective response against pathogens that protects the host from becoming invaded by intruding organisms, thus allowing the body to maintain its normal functioning. In the case of atherosclerosis, excess cholesterol taken up and presented by immune cells may be recognized as such «intruders» and lead to an activation of the immune system. In support of the latter, atherosclerotic lesions show features of chronic inflammation, such as the presence of excessive infiltration of leukocytes in arteries, as well as damage and loss of function of the arterial tissues (6). However, in contrast to an acute inflammation in response to for example infection, in which the immune response will reach a resolution phase once the intruders are defeated, the continued exposure to immune activators in atherosclerosis will induce a chronic inflammation. Hence, atherosclerosis may be viewed as a failed attempt at returning to homeostasis in the long run due to an inefficient resolution of inflammation (6).
Specific receptors on the vascular wall of arteries have been observed to cause the infiltration and migration of inflammatory cells in atherosclerosis (8). Monocytes, a form of leukocytes found in the blood, attach themselves through adhesion molecules on the endothelial lining of the arteries, and are transferred into the tunica intima, the inner arterial layer. Subsequently, stimulating factors make the monocytes differentiate into macrophages within the subendothelial environment (5). These macrophages will take up oxygenated cholesterol and low density lipoproteins (LDL), and eventually become what is referred to as foam cells due to their structure and high lipid content (6). These cells form the core of the developing plaque, together with an extracellular matrix such as collagen, elastin and proteoglycans (8). The phagocytic foam cells also interfere in inflammation by assembling inflammatory mediators in the plaque that can promote inflammation, thereby contributing to the progression of lesions (8).
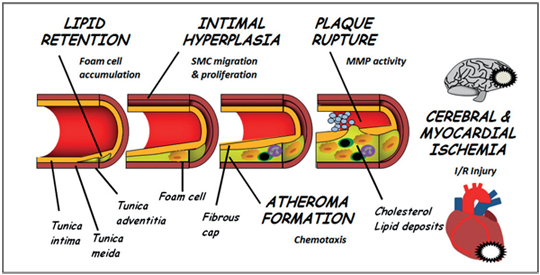
Fig 1: A cross section of an artery, showing the tunica intima (inner layer), tunica media (middle layer) and adventitia (outer layer). This figure also illustrates a developing atheroma formation, with foam cells inside the area containing cholesterol and lipid deposits under the fibrous cap. The final step is a rupture in the fibrous cap of the intima, which is caused by matrix metalloproteinases (MMP activity). Figure adopted from (9).
During the initiation of atherosclerosis, smooth muscle cells (SMC) from the tunica media, the middle layer of the arterial wall, migrate to the tunica intima (9). Some foam cells and SMC die in the plaque cavity leading to the formation of hardened plaque in the arterial wall, which may further lead to stenosis of the arterial lumen. The endothelial cells and the migrated SMC that lay outside the plaque cavity in tunica intima comprise what is referred to as the fibrous cap (Fig. 1). A rupture in this fibrous cap will expose the hard plaque content to the blood flow, leading to platelet activation that triggers the formation of a thrombus, which may occlude the entire vessel lumen and prevent blood flow. This will lead to ischemia of the tissue supplied by the vessel in question, and if this takes place in a coronary vessel, a myocardial infarction will occur. Hence, the rupture of the fibrous cap represents a transformation of the chronic atherogenesis into an acute coronary, cerebrovascular or peripheral extremity ischemic event. The exact cause of the plaque rupture remains to be established, although the instability of the plaque may be due the damaging of proteins in the fibrous cap caused by different proteases that break down the extracellular matrix such as the group of enzymes referred to as matrix metalloproteinases (MMP) (10).
In addition to elevated LDL cholesterol, C-reactive protein (CRP) levels are also increased in people who are at risk of CVDs (11). CRP is an acute phase protein synthesized in the liver in response to inflammation. When a patient has an acute inflammation, the CRP attains high levels, but under normal conditions it is expected to be between 0–5. The CRP level has been suggested to be one of the strongest predictors for identifying patients with a high risk of atherosclerosis. If a person has a constant CPR of 4, this may indicate a low-grade chronic inflammation, and may alert for the incidence of atherosclerosis (11). For this reason, CRP can therefore be seen as a major cardiovascular risk marker, and it has also been demonstrated that there is a strong correlation between CRP level and the risk of myocardial infarction, arterial disease, stroke and sudden cardiac death for both men and women (12).
Current treatments
It is well-known that an unhealthy lifestyle increases the risk of CVD. Factors such as smoking, hypertension, a high cholesterol diet, a low level of exercise and obesity increase the risk for disease. From an epidemiological point of view, a risk factor is a feature of a population or an individual that is recognized at an early stage in life as being associated with an increased risk of developing diseases in the future (12). If patients with established coronary heart disease quit smoking, they lower their death risk by 30–50 % (4). Cessation of cigarette consumption is the most important intervention in preventative cardiology, as smoking has unfavourable effects on blood pressure, reduces myocardial oxygen supply and accelerates atherosclerotic progression (12). Long-term addiction may also increase the oxidation of LDL cholesterol (12). Blood pressure control is also important since it has been demonstrated that hypertension increases the risk of stroke, vascular mortality and general heart failure. The targeted blood pressure should be less than 140/90 mm Hg for the general population, and it has been shown that reductions as small as 4–5 mm Hg significantly reduce the risk of these incidences. Being overweight is also a factor that increases blood pressure, so by exercising, eating a healthy diet with low LDL cholesterol levels and consuming no or low amounts of alcohol, the level of hypertension is expected to go down. High blood pressure is also treated with medication. Patients with high total cholesterol and/or high LDL-cholesterol levels should be treated with lipid lowering drugs (4).
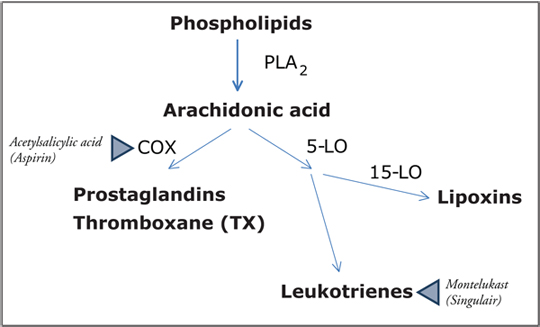
Fig. 2: Arachidonic acid is released from phospholipids by the enzyme phospholipase A2 (PLA2). The formation of prostaglandins and thromboxanes is derived from the cycloxygenase pathway (COX). Leukotrienes are derived from the 5-lipoxygease pathway (5-LO), while lipoxins are derived through the 5-LO and 15-LO pathways. The blue triangles indicate drugs targeting these pathways. Aspirin is a COX-inhibitor used to inhibit thromboxane-induced platelet aggregation, whereas montelukast is a leukotriene receptor antagonist currently used in the treatment of asthma.
Statins, a group of cholesterol-lowering drugs that are widely used in the treatment of CVDs, have been proven to be efficacious in the secondary prevention of cardiovascular events. In addition, statins have been reported to lower CRP levels (13), and experimental observations suggest that statins may also have an effect on immunological reactions and inflammatory processes (14). For example, statins stabilize carotid plaque, and delay the progression of atherosclerosis through anti-inflammatory effects in atherosclerotic rabbits (15). In 2008, it was revealed by a large randomized controlled study called JUPITER that for healthy subjects with elevated CRP levels, rosuvastatin significantly helped in reducing the incidence of major cardiovascular events (13).
The use of acetylsalicylic acid (Aspirin) in the prevention of CVDs has been well established and relies on the inhibition of thromboxane A2 (TXA2), which is a member of the prostaglandin cascade and a potent prothrombotic mediator through platelet activation. This lipid mediator is synthesized from arachidonic acid through the cyclooxygenase (COX) pathway (Fig. 2). Targeting TXA2 through the common low-dose acetylsalicylic acid treatment for the prevention of thrombosis relies on the irreversible inhibition of the COX-1 subtype enzyme in platelets, which lacks the ability to resynthesize COX enzymes, thus leading to a selective inhibition of platelet TXA2 formation, and the subsequent inhibition of platelet function and prevention of thrombosis formation on atherosclerotic plaque. In contrast, inhibitors of the COX-2 subtype enzyme have been shown to be associated with an increased cardiovascular risk. These findings illustrate the complexity of lipid mediators in atherosclerosis.
Leukotrienes as future treatment targets
In 1982, Bengt I. Samuelsson from the Karolinska Institute in Stockholm, Sweden was one of the three Nobel laureates who were awarded the Nobel Prize in Physiology or Medicine «for their discoveries concerning prostaglandin and related biologically active substances» (16). Prostaglandins (Fig. 2), which have been well-known for a long time, play a role in acute inflammatory response, including the regulation of local changes in blood flow and pain sensation (6). In addition, another discovery was leukotrienes and their role in the biological control system (16). These discoveries have been crucial for contemporary theories on how to tackle the problem of chronic inflammation in atherosclerosis.
Leukotrienes are inflammatory mediators which are derived from the 5-lipoxygenase pathway of arachidonic acid metabolism (Fig. 2) (17). Leukotrienes have specific cell surface receptors, and act as potent leukocyte chemoattractants. Some of these receptors have been recognized in human carotid artery atherosclerotic plaque (17). In other words, the activation of some leukotriene receptors may stimulate inflammatory events, e.g. monocyte recruitment, in the arterial wall (7). Macrophages represent a major source of a specific leukotriene production (LTB4), and since macrophages are differentiated from monocytes through leukotriene receptor activation, this becomes a vicious cycle that accumulates inflammatory activity at atherosclerotic sites [8]. Recent studies have suggested that the inhibition of specific leukotrienes may be a possible therapeutic strategy for atherosclerosis, thereby suggesting leukotriene receptor antagonists as a complement to current treatments of atherosclerosis (17).
In fact, several of the above described reactions that characterize atherogenesis could potentially be induced by leukotriene signalling. In addition to activating immune cells and acting as chemoattractants, leukotrienes also activate structural cells within the vascular wall, and have been implicated in the early stages of atherosclerosis, i.e. endothelial dysfunction and intimal hyperplasia (cf. Fig 1). Finally, through the activation of matrix metalloproteinases, leukotrienes could also be involved in plaque rupture.
In support of a major role of leukotriene signalling in cardiovascular disease, inhibiting leukotriene signalling in different animal models has shown beneficial effects. Leukotriene receptor antagonists protect against atherosclerotic lesion development in hyperlipidemic mice, and reduce the intimal hyperplasia response after vascular injury (5). Nevertheless, negative animal studies have also been published in which leukotriene synthesis inhibitors had no effect on atherosclerosis development (5).
In humans, genetic association studies have identified several genes encoding various components of the leukotriene pathways as being associated with atherosclerosis and increased cardiovascular risk. For example, polymorphisms within the 5-lipoxygenase gene were linked to an increased thickness of the carotid artery in an initial study, which was followed by the demonstration of haplotypes within the gene encoding the 5-lipoxygenase activating protein that were associated with an increased risk of myocardial infarction and stroke. However, some contradictory findings exist in terms of the association of cardiovascular disease with genetic variations within the leukotriene pathway, as reviewed in (5).
In asthma, a chronic inflammatory disorder which affects the airways, therapeutic agents that prevent the synthesis of leukotrienes have shown indications of being an effective treatment (18). This could suggest a link between the inflammatory conditions of asthma and atherosclerosis, and inhibiting the 5-LO pathway might be a potential treatment option. Randomized controlled studies of montelukast (Singulair), a leukotriene receptor antagonist, have revealed that it has anti-inflammatory properties during the treatment of asthma (19). Both as monotherapy, or in combination with inhaled corticosteroids, studies indicate that montelukast led to an improvement in the symptoms of asthma, lung function, quality of life and the number of asthma exacerbations (19). Interestingly, montelukast also decreases CRP in asthmatics. As previously mentioned, CRP is an established risk factor in atherosclerosis, and experimental studies of animal models of atherosclerosis have in fact indicated beneficial effects when leukotriene signalling has been inhibited (5).
As mentioned above, not all studies point undisputedly to leukotrienes as potential targets in cardiovascular disease. In this context, it is important to stress that the pro-inflammatory leukotriene pathway may be balanced by anti-inflammatory mediators produced through the same biosynthetical pathway. These molecules are referred to as lipoxins (Fig 2), and have been suggested to promote the resolution of inflammation, allowing for inflamed tissue to return to homeostasis (19). For a complete resolution to occur, further leukocyte recruitment must be inhibited and leucocytes must be removed from inflammatory sites.
Conclusion
In summary, combating the problem of atherosclerosis is a vital task for lowering the rate of CVDs on a global level, and there are still areas of the disease that need to be explored before a fully designed medical treatment can be prescribed. Atherosclerosis has been proven to be more than what scientists used to think were only lipid deposits in the arterial wall. Although the importance of inflammation is now widely appreciated, understanding the vast complexity of the disease is crucial for designing anti-inflammatory treatments as a part of CVD prevention. The leukotriene pathway may be one such possible pro-inflammatory pathway, and drugs that target these mediators are already used in the treatment of asthma. However, in the absence of randomized controlled studies of anti-leukotrienes in patients with atherosclerosis, no recommendations can yet be made as to the use of these drugs in CVD prevention. In addition, lipid mediators may have both pro- and anti-inflammatory properties, and a complete understanding of these pathways in atherosclerosis still remains to be established.
Literature
http://www.who.int/mediacentre/factsheets/fs317/en/index.html
Dahlof, B., Cardiovascular disease risk factors: epidemiology and risk assessment. Am J Cardiol, 2010. 105(1 Suppl): p. 3A-9A.
http://statbank.ssb.no/statistikkbanken/Default_FR.asp?PXSid=0&nvl=true&PLanguage=0&tilside=selectvarval/define.asp&Tabellid=03309
Wallentin L., Lindahl B. Akut kranskärlssjukdom. Liber, 2010, ISBN 978–91–47–09388–5.
Bäck, M. Inhibitors of the 5-lipogenase pathway in atherosclerosis. Current Pharmaceutical Design 2009; 15: 3116–32.
Spite, M., Serhan, C.N. Novel lipid mediators promote resolution of acute inflammation: impact of aspirin and statins. Circ Res. 2010 Nov 12;107(10):1170–84.
Bäck, M., Hansson, G.K. Leucotrine receptors in artherosclerosis. Annals of Medicine 2006; 38: 493–502.
Libby, P., Ridker, P.M, Hansson, G.K. Progress and challenges in translating the biology of atherosclerosis. Nature 2011: May 19;473(7347):317–25.
Bäck, M. Leukotriene signaling in atherosclerosis and ischemia. Cardiovasc Drugs Ther. 2009 Feb;23(1):41–8.
Bäck, M., Ketelhuth, D.F., Agewall, S. Matrix metalloproteinases in atherothrombosis. Prog Cardiovasc Dis 2010;52:410–428.
Ridker, P.M., Rifai, N., Rose, L., Buring, J.E., Cook, N.R. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002 Nov 14;347(20):1557–65.
Zipes, D.P., Libby, P., Bonow, R.O., Braunwald, E. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. Seventh Edition. 2005. Vol 1.
Ridker, P.M., Danielson, E., Fonseca, F.A., Genest, J., Gotto, A.M. Jr., Kastelein, J.J., Koenig, W., Libby, P., Lorenzatti, A.J., MacFadyen, J.G., Nordestgaard, B.G., Shepherd, J., Willerson, J.T., Glynn, R.J.; JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008 Nov 20;359(21):2195–207.
Bu, D.X., Griffin, G., Lichtman, A.H. Mechanisms for the anti-inflammatory effects of statins. Curr Opin Lipidol. 2011;22:165–70.
Zhou, G., Ge, S., Liu, D., Xu, G., Zhang, R., Yin, Q., Zhu, W., Chen, J., Liu, X. Atorvastatin reduces plaque vulnerability in an atherosclerotic rabbit model by altering the 5-lipoxygenase pathway. Cardiology 2010;115(3):221–8. Epub 2010 Mar 16.
http://nobelprize.org/nobel_prizes/medicine/laureates/1982/samuelsson.html
Bäck, M., Bu, D.X., Bränström, R., Sheikine, Y., Yan, Z.Q., Hansson, G.K. Leukotriene B4 signaling through NF-kappaB-dependent BLT1 receptors on vascular smooth muscle cells in atherosclerosis and intimal hyperplasia. Proc Natl Acad Sci USA 2005 Nov 29;102(48):17501–6.
Drazen, J.M. Asthma therapy with agents preventing leukotriene synthesis or action. Proc Assoc Am Physicians 1999 Nov-Dec;111(6):547–59.
Diamant, Z., Mantzouranis, E., Bjermer, L. Montelukast in the treatment of asthma and beyond. Expert Rev Clin Immunol. 2009 Nov;5(6):639–58.
medical student, University of Copenhagen, Denmark
gsw294@alumni.ku.dk (corresponding author)
MD, MSci, Karolinska Institutet, Stockholm, Sweden
MD, PhD, Associate Professor of Cardiology, Karolinska University Hospital,
Stockholm, Sweden
