Latvian health
In a way, the diagram on tuberculosis incidence 1985–2003* See also Siem 2004. summarizes the whole story about Latvian health in the years of transition: Two simultaneous developments have been running side by side. One process has been running down the road to economic growth and prosperity, the other on the road to a worsening general health condition in the population.
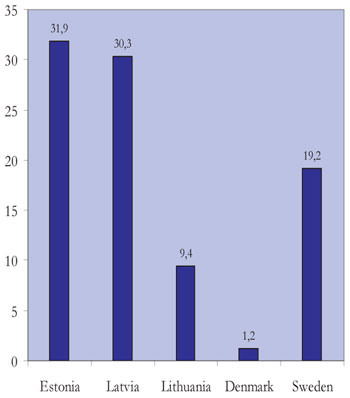
A closer look at the tuberculosis figures shows that Latvia is even among the weakest guys of the class when Baltic Sea countries are compared, only sharing this dubious honour with the Russian Federation. Especially for the years around 2000, the incidence numbers were very high, e.g. exceeding Nordic averages by a factor of approximately ten.
Admittedly, declining incidence curves, in the most recent years, indicate a positive, yet still ongoing development with much room for catching up. However, the reasons for that new trend remain to be discussed, and the final clues will not be visible until several further years have elapsed. When it comes to infectious diseases like tuberculosis, the effect of national and international initiatives, of course, may be at hand, but an assessment of the outcomes of the «Task Force on Communicable Disease Control in the Baltic Sea Region» probably has to be postponed* Hønneland & Rowe 2004. and seen in light of other developments. More likely, the turning the tide is the product of rising living standards and economy, a health care system which has resumed function, and a shift in attitudes connected to the value of preserving health.
The impact of the public health services is more complicated to foresee, as the abandoned Soviet health care system, in general, placed considerable weight on preventive measures. System-based preventive health care activities such as vaccinations and health examinations were mostly unquestioned parts of daily life; although failures could be expected due to lack of optimal resources.
The period of chaos following independence was soon replaced by a large scale adjustment of the society in most areas, to comply with standards set by the European Union as requirements for acceptance of the membership application. It is possible that this broad approach is showing results, as coming to light in the diagram on tuberculosis, but on the other hand a positive tendency is also appearing for the countries of the Russian Federation, where EU issues do not apply. Here, new specific studies will be necessary to assess the reasons and causation behind what has happened.
Tuberculosis incidence in the Eastern Baltic Sea countries per 100 000 inhabitants* Siem 2004..
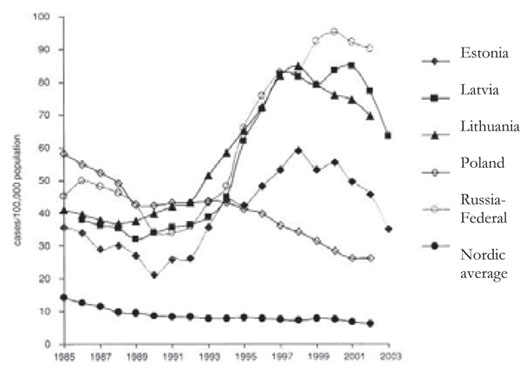
Source: WHO Europe 2004. 2003 data provided by chief epidemiologists.
Note: 2003 data are provisional. Early data for Russia for 2003 give an incidence rate of 70, confirming the positive development.
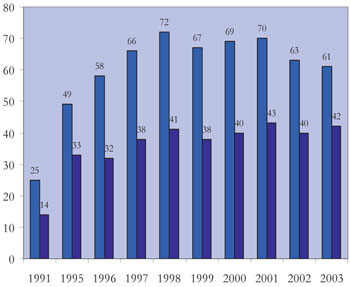
Incidence of tuberculosis in Latvia per 100 000
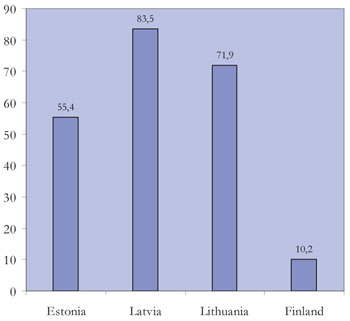
Incidence of tuberculosis per 100 000 in 2002
Viral hepatitis per 100 000 Inhabitants
Incidence of viral hepatitis B per 100 000 by country in 2000
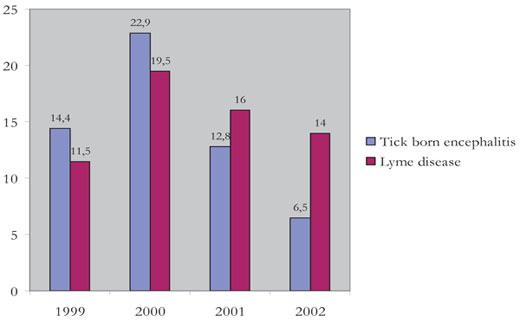
Morbidity from tick borne infections per 100 000
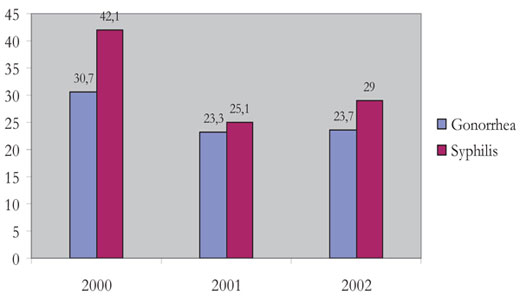
Morbidity from sexually transmitted infections per 100 000
Moorlands west of Riga, a place where mosquitos thrive (2002).
The population at risk for diseases and atrocities and the population exposed to both the deleterious and the health promoting factors of their home society, is in this case the permanent residents in Latvia. The number has been laying quite constantly around 2.5 million; although with a slight decline from 1995 to 2001 and a possible minor upward tendency in 2004.
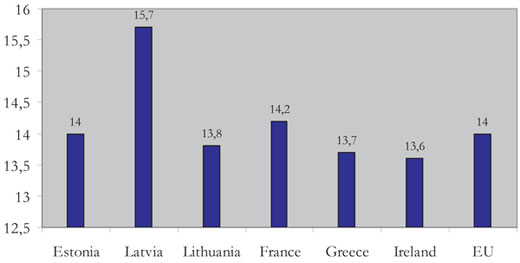
We have already touched upon a Latvian peculiarity – the present sex distribution – as the male population constantly only makes up only around 46 % of the total population. This is reflected in the mortality rate per one thousand inhabitants, which for both sexes taken together was 15,7 in 1995 and 2002. Aside from this, mortality has fluctuated slightly around 14 since 1996, which equals the EU average for 2002 – as far as the national health statistics can be trusted.
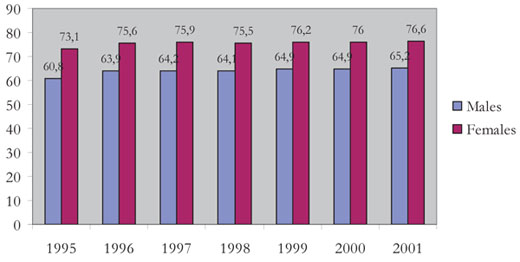
The sex difference appears in the average life expectancy. For males it was 60,8 years in 1995, contrasting a female life expectancy of 73,1 years, a difference of 12,3 years. By 2004, the corresponding figures were 67 and 78,2 years respectively. The sex difference of 11,2 years means a reduction in the difference by 1,1 years.
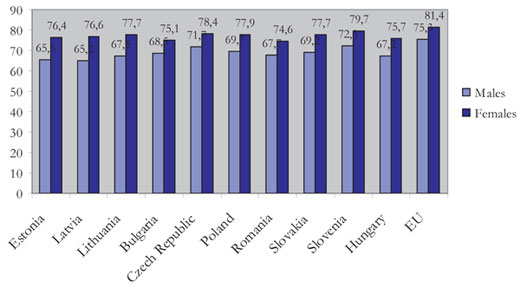
This of course is positive, but if seen by country in 2000, Latvia is still worst off with an 11,4 years difference between the sexes. The EU average, then of course excluding Latvia, was 6,1 years with 81,4 years for females and 75,3 years for males. However, the population has changed in age composition: Throughout the 1990s the under 18 years age group diminished by some 3 %, and a corresponding increase of the same size could be seen for the 65+ group.
The major causes of mortality, both sexes taken together, has a pattern familiar to many countries: diseases of the circulatory system hold the top ranking of 56,0 per cent in 2003 and tumours 17,4 per cent the same year. However, 11,3 per cent of deaths caused by injuries, intoxication and external causes in 2003 is a matter of concern. Looking into the most common causes for hospitalization, diseases of the circulatory system make up 15,2 % and are followed by injuries, intoxications and external causes at 11 % in 2002.
Road traffic has to take its share of the responsibility here, as accidents of course will be a risk in a country where extensive private car ownership is something new. Alcohol consumption is a factor of major interest in this respect. Alcohol consumption in Latvia has decreased slightly between 1994 and 2000 (7,6 to 6,9 litres of pure alcohol per capita per year), but in 2000 it is still much lower than in Denmark (9,5 litres per year) and equals the consumption in Finland. So there should also be alternative explanations to be sought in the discussion of health differences and developmental tendencies over time.
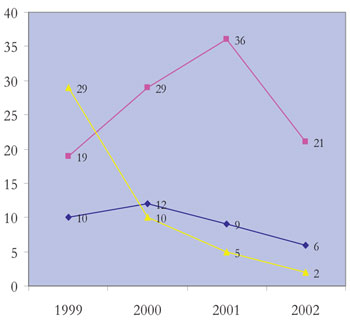
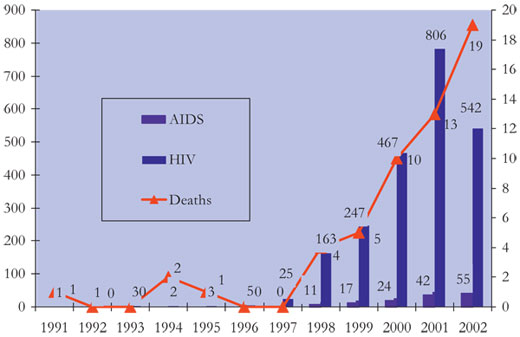
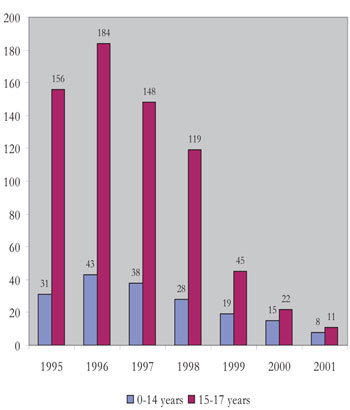
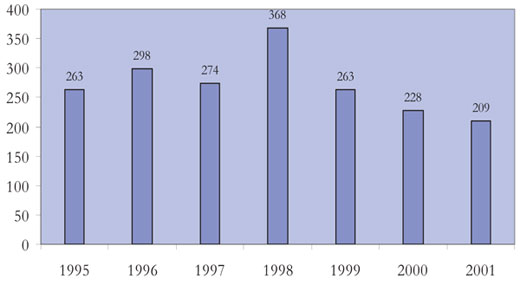
New and deleterious health behaviour in the years following independence may be seen from the statistics for spread of HIV-infection and AIDS. In 1991 this problem was almost non-existing. Even if the numbers ten years later are still low, an increase at an almost exponential pace should cause concern about sexual behaviour and drug abuse and spark preventive measures. However, what these figures do not tell, is about the extent of change in habits. They only document the infection by an agent obviously brought into Latvian society a short time ago. This fact should be taken into account when staging the counteracting strategies: Avoiding the viral infection is obviously the core of the question. As shown in the diagram on syphilis among young people, figures have decreased. Although figures are diminishing, they have to be interpreted with caution due to possible fallibilities of the reporting system.
Spread of HIV infection in Latvia (cases)
|
Abortions per 1000 live births |
Latvia |
734 |
Estonia |
834 |
Lithuania |
416 |
Finland |
196 |
Sweden |
348 |
The diagram illustrating the occurrence of diphtheria during the same years points at another type of infection hazard following independence: The strong vaccination regimes were made more lax, and the effect of a situation when the population was only partly covered by vaccine popped up like a showpiece: Two epidemics with peaks in 1995 and 2000 became the proof that freedom should not be freedom from everything, such as from vaccination regimes. A pity for those who were hurt but a lesson for all the others.
When discussing Latvian health there is a special feature which deserves to be mentioned – the high morbidity of tick borne encephalitis. An explanation is to be found in the landscape of the whole Baltics. As seen on our aerial photograph there are widespread areas with glades and swamps, excellent ecosystems for insects in hot and humid summers, making the popular pastime of mushroom and berry picking risky.
Diagrams, tables and flowcharts on the reorganisation of the health care services demonstrate that a new structure with potential for good function has indeed emerged. One of the big problems, however, apart from the finances, has been the rapid and frequent changes and adjustments in the setup which has hampered the implementation and settling in of the system.
As can be extracted from statistics, around half of the doctors currently serving in primary health care are general practitioners in the Scandinavian sense – supplemented by paediatricians and interns. The number of beds in hospitals is decreasing, mostly reflecting new treatment protocols with shorter stays.
Cockerham (1999) discussed in depth the relationship between health and social change in Russia and Eastern Europe. In his concluding chapter he resumed his analyses of the two main principles seen in the health services in the world: the socialist and the capitalist. The socialist approach, he wrote, was to co-opt health care as a state commodity, paid for centrally and offered for free. One of the disadvantages of this system, which at first sight may seem both just and caretaking, is that health care never materializes directly in results which add to the prime goals of production of the traditional communist countries, and thus lose priority and may subsequently suffer from underfinancing.
Incidence of syphilis among children and adolescents (number of cases)
On the other hand, the capitalist approach is in its principle a fee-for-service system. The fact that national health service programmes have been set up in Western welfare states, perhaps conceals the capitalist nature of the services. Even the most elaborate Western welfare system is based on fee-for-service, even if there are built-in mechanisms which reduce or eliminate the part of the payment to be covered by the patient.
One might say that the socialist health care system took over responsibility from the individual, expecting loyalty, equity and equality in return. Its weakness originated in the failure in keeping the promises such a responsibility implied.
On the other hand, the capitalist health care system can be said to be unjust in nature: The responsibility for health is basically placed on the individual itself, disregarding individual abilities to take it over. Although the individuals in these types of societies as a rule have long traditions in organising themselves in ways which secure mutual safety, the inequality and inequity might bluntly be claimed to be fundamentals of capitalism and market economy. Welfare redistribution systems have as their basic aims to counteract, not to remove inequality and inequity. Thus they also may be accused of preserving the situation. The diversification of the capitalis system, as already argued by Adam Smith (1723–1790) more than two hundred years ago simply has inequality as an inherent trait, to which inequity adds on more philosophical and cultural grounds.
A principle running in parallel is charity. Charity in the sense of sharing your assets with others, fits into purist communist ideology, but is also in line with most religions and moral philosophies. However, charity in a capitalistic freemarket setting may also be accused of maintaining class differences by visualising the separation between the needy and the affluent and giving the affluent the upper hand in their capacity to decide over the distribution of assistance on their own terms. Charity fulfils needs both on the side of the recipient and the provider. Even when non-governmental organisations (NGOs) are recruited by the authorities as collaborative partners in providing welfare and health care, there is a risk of maintaining the status quo, by targeting the symptoms, not the cause of inequality and inequity. The same objection can be applied to the traditional social medicine approach in public health. To help underprivileged groups and to develop knowledge and tools to do so, is both necessary and appropriate. There is a danger, however, that interests and efforts are diverted away from a public health approach that is directed against the causes of the misery, and the cause may lie far outside thT which normally is perceived as within the medical sphere* See Larsen “Exploring external and internal public health concepts” (2004); Tellnes “The community approach to public health” (2004), Mittelmark “New objectives in public health” (2004) and Aarsæther “Reflections on health and democracy” (2004)..
The Moscow suburb, Riga (2002).
In the case of Latvia, a transition between the two totally different systems had to take place in years when similar transitions were going on simultaneously in almost all other areas of society. As discussed by Aage (1998), in his comparison of the Baltic and the Nordic countries, during the same years Latvian economy experienced an almost disastrous setback, with a gross domestic product in 1995 only arriving at 50,5 % of the 1989 level. People often had a really hard time and suffered as a result, a situation which would normally call for ample assistance from a well-functioning health service which simply was not there.
To make it even more complicated, the whole notion of health was also in transition. The cultural shift in Western medicine towards greater medical attention to the perceived morbidity, the experience of being ill, became present over time also in Latvia, widening the expectations to the care given by the health services, particularly in primary health care* For a review of the different faces of morbidity, see e.g. Larsen 2005.. The failing health care and the still weak public health system not only had to go through a process of restoration, but a shift in objectives and a widening of tasks also had to be faced.
Still, it is too early to know how the health reforms have worked out. Building up a primary health care system in Latvia has been a prime issue, including a patient list principle. By 2001 we set up a study to see how people perused this offer of a physician’s services* See Kilkuts & al. 2004 (I).. 948 adult Latvians were chosen by chance in five practices and compared to 1037 Norwegian patients. In the Latvian population at that time, the general reasons for seeing a doctor were much the same as in Noway. But there were a higher proportion of respiratory and gastrointestinal illness amongst the Latvians than amongst the Norwegians. In addition, the clinical practice was also a little bit different: The tendency to prescribe antibiotics for common infections was high in Latvia, and a significant proportion of the doctors involved admitted that they felt under pressure from patients to prescribe them. This fact is a cause for concern in comparison with the general reluctance to prescribe antibiotics, when not absolutely needed, elsewhere in Europe, because of the resistance problem.
Another point coming out of a parallel study* See Kilkuts & al. 2004 (II)., with informants from the same material, showed that more than a half of the patients regarded themselves as having a substantial risk of attracting contagious disease. But the belief in treatment, for example by antibiotics, was stronger than the belief in prevention. This finding indicates that prevention should be tailored: A change in attitudes and in risk perception is probably required.
Mortality rate in Latvia (‰)
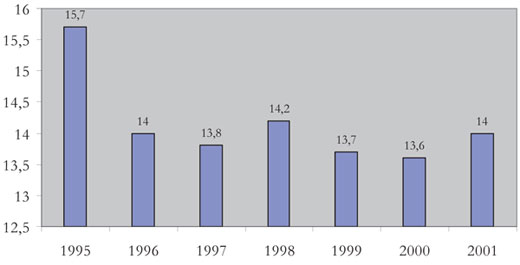
Mortality rate by countries (‰)
Average life expectancy in Latvia (years)
Average life expectancy by country (2001)
Deaths from injuries related to alcohol abuse
Incidence and mortality of malignant tumours per 100 000
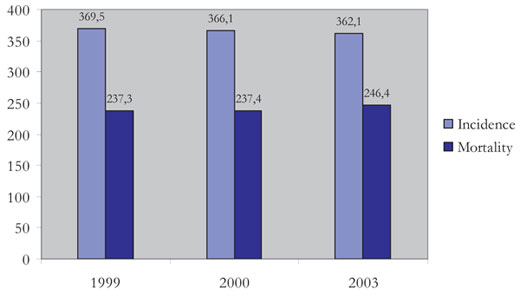
Most common malignant tumours for females and males (2001, per cent)
|
2000 |
2001 |
2002 |
Visits to doctor (per 1 person) |
4.8 |
4.8 |
4.5 |
Tuberculosis morbidity (per 100 000 population) |
72.3 |
73.4 |
65.4 |
|
41.1 |
43.7 |
40.9 |
Diagnosis of malignant tumors: |
|||
|
24.3 |
26.0 |
23.9 |
|
29.4 |
32.6 |
30.0 |
Incidence of malignant tumors in prophylactic checks (%) |
1.8 |
1.2 |
1.6 |
Operations (per 100 000 population) |
|||
|
25.7 |
26.4 |
22.7 |
|
9.7 |
9.4 |
6.8 |
Alcohol psychosis (occurring for the first time) per 100 000 |
41.0 |
39.0 |
35.6 |
Mortality (per 100 000 population) |
|||
|
517.5 |
553.3 |
557.8 |
|
15.4 |
14.9 |
15.0 |
|
6.4 |
6.3 |
5.8 |
|
11.7 |
11.9 |
9.0 |
Mortality of mothers (per 100 000 live born) |
24.8 |
25.4 |
10.0 |
Mortality of infants (o/oo) |
10.4 |
11.0 |
9.9 |
Perinatal mortality (o/oo) |
12.1 |
12.3 |
12.6 |
These results confirmed our hypothesis that the prevailing risk perception is a key both to understanding and to intervention. A more extensive study was originally planned, but different circumstances made it necessary to limit the ambitions.
The picture of primary care encounters of 2001 should also have been supplemented by longitudinal studies. However, there is the general impression that stress and anxiety have become gradually more important among patients, as time has gone by. Figures and other hard facts supporting this, could not be established, but a theory is that the many choices and the ever present ambiguity and unaccustomed insecurity of the modern society have become a problem difficult to cope with for many individuals.
This is the background of the figures and diagrams and the text of this chapter on Latvian health in the years of transition. Most interest among researchers has been concentrated on the factors impairing health* E.g. Cockerham 1999.. Living through the same years in the Latvian society and having daily contact with people’s health makes the Latvian author of this chapter pose the question the other way round: Why wasn’t it worse? Which hidden forces made the Latvians maintain a certain level of health and restore a health care system against a myriad of odds? And the Norwegian author may wonder what impact all the influence from the outside world may have had: From sensible and serious assistance programs to relief with hidden agendas.
Riga Central Market hall 1993.
and
